Birth Control: The Basics
Birth control, also known as contraception, helps prevent pregnancy. There are a variety of different types of birth control, each coming with its own set of risks and benefits. Barrier methods, such as male and female condoms, help prevent pregnancy by blocking sperm from entering the uterus; however, this method tends to have a lower effectiveness compared to other birth control methods. Hormonal methods, such as oral contraceptives, help prevent pregnancy by stopping ovulation. Preventing ovulation stops the release of an egg from the ovary, which prevents pregnancy by preventing egg fertilization.
As of 2019, 48% of women of reproductive age (15-49) worldwide use birth control; 44% of these women use modern contraceptive methods and 4% use traditional methods of birth control such as withdrawal and rhythm methods (United Nations, 2019).
Birth control has benefits beyond pregnancy prevention. Oral hormonal contraceptives offer many therapeutic benefits for a variety of conditions. Hormonal contraceptives have helped treat a variety of disorders such as menstrual bleeding disorders and endometriosis. Birth control is also used as a therapeutic agent to prevent conditions such as ovarian cysts and pelvic inflammatory disease (Schindler, 2012).
EFFECTIVENESS
Experts often refer to typical use failure rate to assess the effectiveness of a birth control method. Typical use failure rate for contraception refers to the failure rate of preventing pregnancy from all users, which includes individuals who incorrectly or inconsistently used the contraceptive method. The effectiveness of each method varies for a variety of reasons and typical use failure rate can help inform decision-making (Guttmacher Institute, 2020).
TYPES OF BIRTH CONTROL
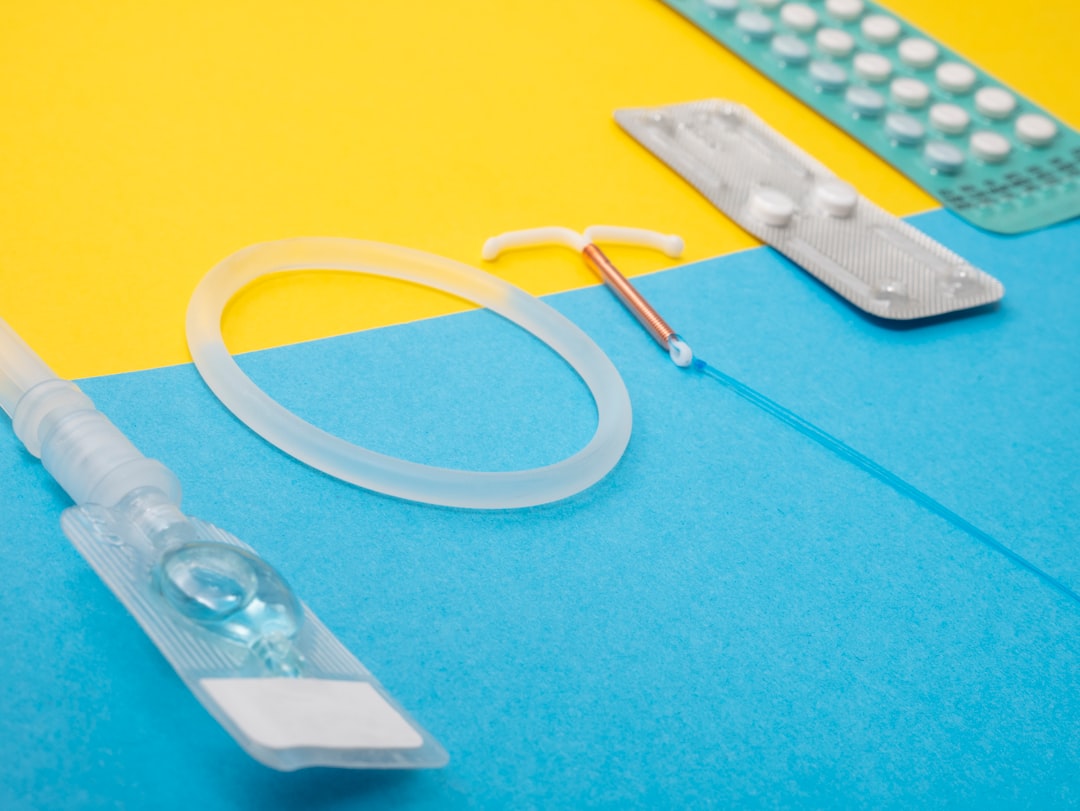
There are a variety of different birth control methods including: intrauterine contraception, hormonal contraception, barrier methods, fertility awareness-based methods, lactational amenorrhea method, emergency contraception, and sterilization.
INTRAUTERINE CONTRACEPTION
Intrauterine contraception consists of two different devices: the levonorgestrel intrauterine system (LNG IUD) and the copper T intrauterine device (copper IUD). The LNG IUD is a hormonal contraceptive that releases a small amount of progestin each day to prevent pregnancy. Progestin is a synthetic form of progesterone, a hormone involved in the menstrual cycle (Edwards and Can, 2022). The IUD can stay within the uterus for 3 to 6 years and has a typical use failure rate of 0.1-.4% (Centers for Disease Control and Prevention [CDC], 2022). The copper IUD, or ParaGard, is a non-hormonal IUD. The copper coiled wire on the IUD prevents pregnancy by producing an inflammatory reaction that is toxic to sperm and eggs (Mayo Clinic, 2022). This device can stay in the uterus for up to 10 years and has a typical use failure rate of 0.8% (CDC, 2022).
HORMONAL CONTRACEPTION
There are a variety of different hormonal contraception methods. The implant is a form of contraception that is inserted under the skin and prevents pregnancy by releasing progestin into the body over a three year period. The typical use failure rate of the device is 0.1%. The contraceptive method called Depo-Provera is a progestin injection given every three months with a typical use failure rate of 4%. There are two different types of oral contraception: combined oral contraceptives, which contain both estrogen and progestin, and a progestin-only pill. Both forms of oral contraceptives have a typical use failure rate of 7%. Additionally, a patch can be placed on the skin to release progestin and estrogen into the bloodstream. This device must be changed each week for three weeks and has a typical use failure rate of 7%. Lastly, a hormonal vaginal contraceptive ring is a device placed inside the vagina for three weeks. The device releases progestin and estrogen and has a typical use failure rate of 7% (CDC, 2022).
BARRIER METHODS
Barrier methods are used to prevent pregnancy by preventing sperm from entering the uterus.
Diaphragm: A diaphragm or cervical cap can be inserted into the vagina to cover the cervix. This method has a typical use failure rate of 17%. Sponges containing spermicide, a chemical that kills sperm, is inserted in the vagina to cover the cervix and block sperm.
Sponge: The sponge works for up to 24 hours and must remain in the vagina for at least six hours after intercourse. The typical use failure rate for this device is 14% for women who have never had a baby and 27% for women who have had a baby.
Male and Female Condom: Male condoms are another form of a barrier contraceptive and in addition to pregnancy prevention, condoms also help prevent STDs. Male condoms have a typical use failure rate of 13%. Female condoms are a less commonly used barrier method which are less effective than male condoms and have a typical use failure rate of 21%. This method can be left in the vagina for up to eight hours before intercourse. Spermicides can be used as a contraceptive method alone or with other barrier methods. If used alone, spermicides have a typical use failure rate of 21% (CDC, 2022).
FERTILITY AWARENESS-BASED METHODS
Fertility awareness-based methods, commonly known as rhythm methods, is a method of birth control that uses fertility patterns to prevent pregnancy. Fertility pattern refers to the number of days in the month when an individual is fertile, infertile, and when fertility is unlikely (CDC, 2022). This method requires the user to track certain signs and symptoms, such as menstrual cycle length, basal body temperature, urinary hormone measurements, and cervical fluid, which change during the fertile window and menstrual cycle (Simmons and Jennings, 2020). If the user has a regular menstrual cycle, they can use barrier methods during fertile days or avoid intercourse to prevent pregnancy.
LACTATIONAL AMENORRHEA METHOD
Lactational Amenorrhea Method (LAM) uses three different indicators to measure fertility and prevent pregnancy. After a recent pregnancy and while breastfeeding, LAM can be used as birth control if the individual is not currently menstruating, fully or nearly fully breastfeeding, and is less than six months postpartum. During this period, breastfeeding temporarily presents ovulation and thus prevents pregnancy (CDC, 2022).
EMERGENCY CONTRACEPTION
Emergency contraception is used to prevent pregnancy after unprotected intercourse. The copper IUD can serve as emergency contraception if inserted within five days of unprotected intercourse. Emergency contraceptive pills, such as Plan B, can also be taken up to five days after unprotected sex to prevent pregnancy (CDC, 2022). Emergency contraceptives can prevent up to 95% of pregnancies if taken as recommended (World Health Organization, 2021).
PERMANENT METHODS OF CONTRACEPTION
Lastly, there are more permanent methods of birth control. Female sterilization, or tubal ligation, is a procedure where the fallopian tubes are tied to prevent fertilization and pregnancy. The typical use failure rate for this method is 0.5% Male sterilization, also known as a vasectomy, is a male sterilization procedure that prevents sperm from reaching the semen by blocking the vas deferens tube. The typical use failure rate of this procedure is 0.15% (CDC, 2022).
Lifestyle
NUTRITION AND SUPPLEMENTS
In terms of nutrition, there is inconclusive evidence that women on birth control need vitamins and supplements. The vitamins and minerals assumed to be required by women on birth control are vitamins B-6, folic acid, riboflavin, vitamin C, and vitamin A, zinc, iron, and copper. It’s difficult to detect exact levels of these vitamins in the blood stream of women on birth control, however it is recommended that women on oral contraceptives follow a healthy and balanced diet rich in vitamins and minerals (Nutrition and Oral Contraceptives., 2010).
VITAMINS
Vitamin B-6: Vitamin B-6 (Pyridoxine), is an important vitamin for normal brain development and for a healthy immune system. Vitamin B-6 is found in fish, poultry, meat, whole grains, potties, sweet potatoes, and brewer's yeast. Vitamin B-6 can be taken as a supplement available as an oral capsule, tablet or liquid (Mayo Clinic., 2021).
Folic acid: Folate (vitamin B-9) is important for the formation of red blood cells and healthy cell growth and function. Folate is extremely important during the early stages of pregnancy to reduce the risk of birth defects of the brain and spine. Folate is found in liver, dark green leafy vegetables, and dried beans (Mayo Clinic., 2021).
Riboflavin: Riboflavin (vitamin B 2) is needed to break down carbohydrates, proteins, and fats Riboflavin is found in milk, meat, poultry, fish, dark green leafy vegetables, grains and cereals (Mayo Clinic., 2021).
Vitamin C: Vitamin C or ascorbic acid is a nutrient needed to form blood vessels, cartilage, muscle and collagen in bones. Vitamin C is also important for cell protection against the effects of free radicals and helps the body with the absorbing and storing of iron. Vitamin C is found in fruits and juices, strawberries, cantaloupe, pineapple, broccoli, peppers, brussels sprouts, spinach, cabbage (Mayo Clinic., 2021).
Vitamin A (retinol, retinoic acid): Vitamin A is important for vision, growth, cell division, reproduction and immunity; it has antioxidant properties which help protect the cells against free radicals. Vitamin A can be found in green leafy vegetables (spinach, turnip topic, chard, beet greens), green stem vegetables (asparagus, broccoli), yellow vegetables (carrots, sweet potatoes, winter squash), yellow fruits (apricots, peaches, cantaloupe) (Mayo Clinic., 2021).
MINERALS
Zinc: Zinc is a nutrient found in the body and helps your immune system and metabolism. Zinc can be found in oysters and other seafood, meat nuts, and whole grain breads (Mayo Clinic., 2021)
Iron: Iron helps red blood cells carry oxygen through the body. If the body does not get enough iron, it cannot produce normal red blood cells. Iron deficiency is a condition also known as iron deficiency anemia. Iron can be found in meat, poultry, liver, fish, whole grain and enriched cereals and cereal products, dried beans and peas, prune juice, deep green leafy vegetables.
Copper: Copper is an essential mineral, naturally available in some foods and as a dietary supplement. Copper is involved in many physiological processes for example angiogenesis, regulation of gene expression, brain development, immune function and pigmentation. Copper can be found naturally in oysters and other seafood, liver, nuts, dried beans and peas, and dried fruits (Dietary Supplement Fact Sheets., 2021)
EXERCISE
During a natural cycle, women experience fluctuations in mood and overall motivation to engage in physical activity. Women with less predictable menstruation cycles often opt in for an oral contraceptive to regulate their cycle, which in effect will balance out hormones during this phase. In a recent study on athletic performance by women on oral contraceptives compared to women in a normal cycle, results showed that “performance was consistent across the 28-day cycle” in comparison to women in a natural cycle (SportsMed., 2020). This study suggests that athletic performance can be “masked” by the effects of oral contraceptives, which can help with hormonal imbalance and peak performance capacity.
SEXUAL HEALTH
Choosing a method of contraception there are several key factors to consider: safety of the product, its effectiveness, and availability (accessible and affordable). To understand these key factors, it is important to receive medical guidance from a primary care provider to fully understand the product and how to use it. Furthermore, the use of contraception and taking steps to protect against HIV and other STDs must be considered. While contraceptives can be effective in preventing pregnancy, they do not protect against STDs. Reduce the risk of HIV infection and other STDs (chlamydia, gonorrhea, and trich) by effectively and consistently using a condom (CDC., 2022).
DRINKING AND SMOKING
There are known risks with both drinking and smoking individually, however the effects of these on an individual taking birth control can bring serious health complications. Smoking on its own can cause strokes and coronary heart disease. It can also damage blood vessels by making them thicker and narrower. The effects of smoking on an individual on birth control are concerning as the estrogen found in birth control pills can promote the thickening of the blood which can be dangerous for a woman who smokes cigarettes (University of Colorado., 2022).
Quitting smoking is the most important step you can take to improve your overall health. If you need help quitting call 1-800-QUIT-NOW.
While there is not substantive evidence that drinking alcohol will impact the effectiveness of birth control. Drinking too much alcohol can hinder a person’s judgment, leading to regrettable decisions. Furthermore, it’s important to be aware of tolerance levels when drinking, and understand that being on birth control does not equate to being fully safe from contracting other diseases (Planned Parenthood., 2015).
HORMONES
Combined hormonal contraceptives (CHCs) are the most common type of contraceptive prescribed. CHCs can be prescribed through a pill, patch, or vaginal ring, in which progestins and estrogen inhibit the hypothalamic-pituitary-ovarian axis that controls the reproductive cycle. The progestins prevent pregnancy by inhibiting the luteinizing hormone surge, and suppressing ovulation, thickening the cervical mucus and lowering fallopian tube motility which in effect cause endometrium to become atrophic (NIH., 2020). Estrogen prevents pregnancy by suppressing follicle stimulating hormone (FSH) production, preventing the development of a dominant follicle. Progestin is responsible for contraceptive action and side effects, furthermore, the additional estrogen helps prevent irregular menstruation (NIH., 2020).
Research We’re Following
MEN’S BIRTH CONTROL
In a recent press release by the American Chemical Society, a group of researchers from the University of Minnesota have developed a non-hormonal male contraceptive that works by targeting a protein called retinoic acid receptor alpha. This protein is in the family of three nuclear receptors that bind to retinoic acid (a type of vitamin A) that plays a significant role in cell growth, differentiation (sperm formation) and embryonic development. In this study, researchers were able to knock out the RAR - alpha gene in male mice, making them sterile. When the mice were taken off the protein, the effects were reversed. At this time, men have two options for contraception, the condom which is single-use and may be prone to failure, and vasectomy, a procedure considered to be a permanent form of male sterilization(ACS, 2022). The paper was presented during the American Chemical Society in the Spring 2022 meeting, clinical trials are expected to begin as soon as 2022, depending on the results of the trial male contraceptives could soon be available.
Resources
APPS AND SERVICES
Clue - Period tracker
Pandia Health - Subscription birth control
PROFESSIONAL ORGANIZATIONS
REFERENCES
“A Non-Hormonal Pill Could Soon Expand Men’s Birth Control Options.” American Chemical Society, ACS Newsroom, www.acs.org
Britton LE, Alspaugh A, Greene MZ, McLemore MR. CE: An Evidence-Based Update on Contraception. Am J Nurs. 2020;120(2):22-33. doi:10.1097/01.NAJ.0000654304.29632.a7
Center for Disease Control and Prevention (2022). Contraception: Birth Control Methods. U.S. Department of Health and Human Services.
Copper - Fact Sheet Health Professionals. Retrieved April 2022.
“Contraception | Reproductive Health | CDC.” CDC.Gov, CDC, 13 Jan. 2022, www.cdc.gov/reproductivehealth/contraception/index.htm.
“Drugs and Supplements - Drugs and Supplements - Mayo Clinic.” Drugs and Supplements, Mayo Clinic, 16 Sept. 2020, www.mayoclinic.org/drugs-supplements.
Edwards M, Can AS. Progestin. [Updated 2021 Sep 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
Elliott-Sale, Kirsty J et al. “The Effects of Oral Contraceptives on Exercise Performance in Women: A Systematic Review and Meta-analysis.” Sports medicine (Auckland, N.Z.) vol. 50,10 (2020): 1785-1812. doi:10.1007/s40279-020-01317-5
Guttmacher Institute. (2020). Contraceptive Effectiveness in the United States [Fact sheet].
Mayo Clinic. (2022). Copper IUD (ParaGard).
“Heavy Periods and Birth Control.” University of Colorado OB-GYN, 25 Apr. 2017, obgyn.coloradowomenshealth.com.
Nutrition and oral contraceptives - extension. (n.d.). Retrieved April 26, 2022, from https://extension.colostate.edu/docs/foodnut/09323.pdf
Office of the Commissioner. “Birth Control.” U.S. Food and Drug Administration, 18 June 2021, www.fda.gov/consumers/free-publications-women/birth-control.
Pisacreta, Emily. “Does Drinking Alcohol Effect How Well My Birth Control Works?” Planned Parenthood, Planned Parenthood, 8 Aug. 2017, www.plannedparenthood.org.
Schindler, A. E. (2012). Non-Contraceptive Benefits of Oral Hormonal Contraceptives. International Journal of Endocrinology and Metabolism, 11(1).
Simmons, R. G., & Jennings, V. (2020). Fertility awareness-based methods of family planning. Best Practice & Research Clinical Obstetrics & Gynaecology, 66, 68–82.
United Nations (2019). Contraceptive Use by Method 2019. United Nations.
World Health Organization. (2021). Emergency Contraception [Fact sheet].
GENERAL DISCLAIMER
It's Fetch is a community that provides a safe space for members to discuss health and wellness topics. We provide access to archived health related content, note the date of last review or update on all articles. No content shared, regardless of date should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
QUESTIONS
For questions on this article, please contact our team at hello@itsfetch.co.